Providing 24/7 sexual assault and domestic violence care in a lockdown
Last year, the Sexual Assault/Domestic Violence Care Centre (SA/DVCC) at Women’s College Hospital (WCH) saw over 650 patients – an average of 2 people per day. But as Ontario went into lockdown due to COVID-19, the centre saw a sharp decline in patient visits.
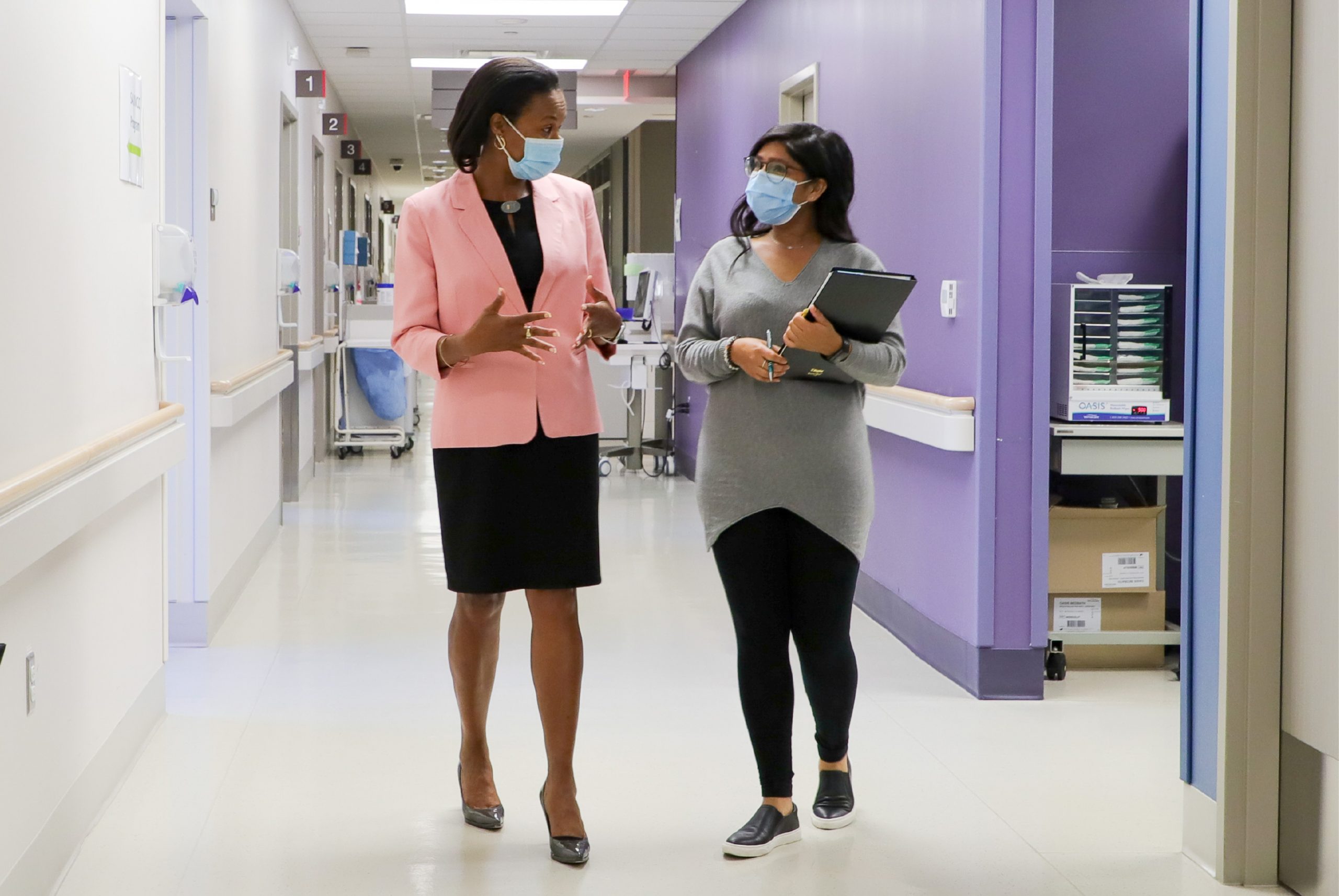
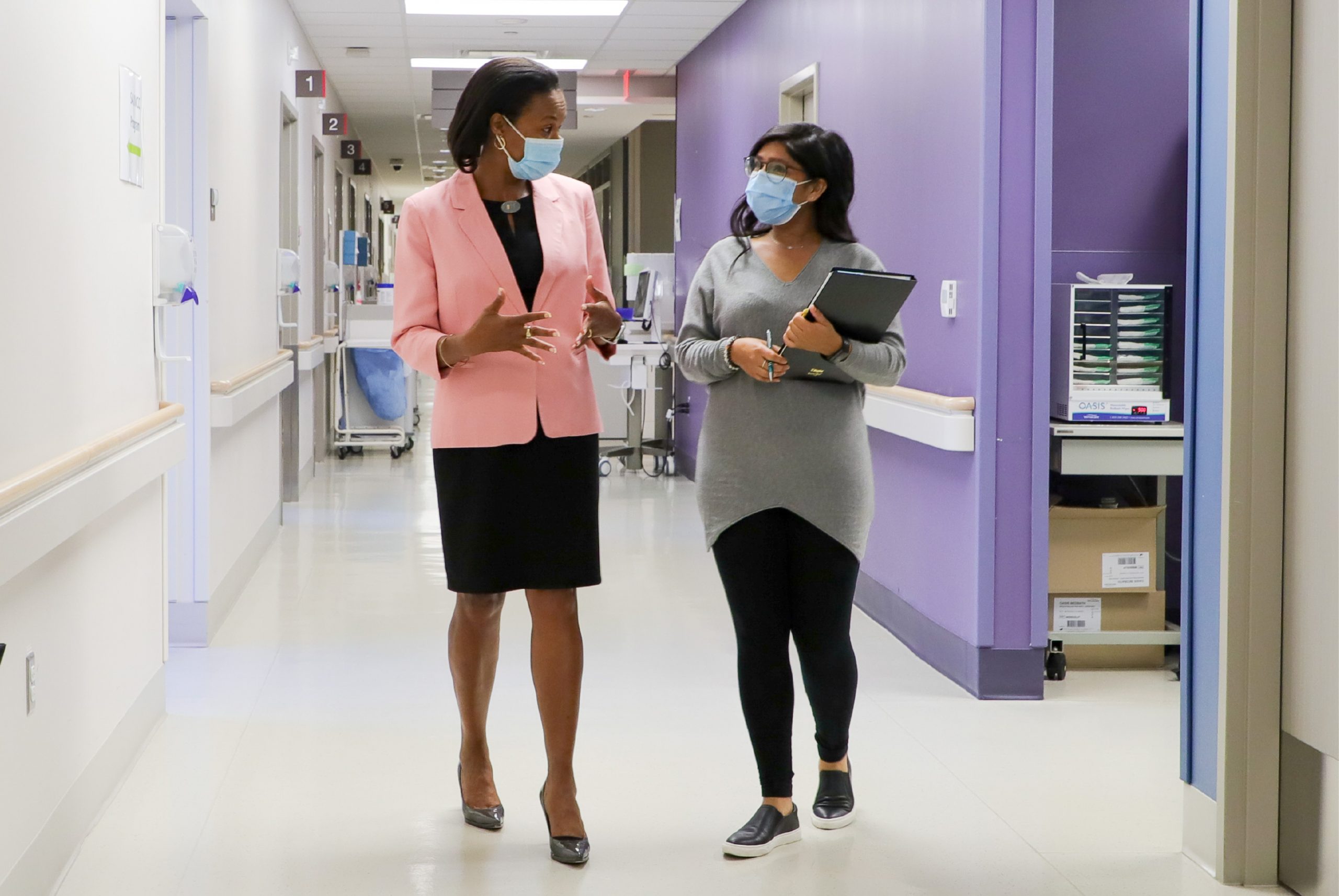
“We always say it would be a great year when we don’t have a single case of sexual assault or intimate partner violence – but this was different,” said Elaine Goulbourne, clinical director of primary care at WCH. “We knew we were seeing the pandemic increase barriers to our care, and this was a great cause for concern.”
Located on the ground floor of WCH, the SA/DVCC is open 24/7 to walk-in patients and also provides mobile services to seven emergency departments in the Greater Toronto Area. The centre aims to provide a safe place and a care plan for those who have experienced sexual assault or intimate partner violence (IPV).
“We knew we were seeing the pandemic increase barriers to our care, and this was a great cause for concern.”
“There are various types of care that we provide,” explained Sukhpreet Kainth, a registered nurse in the SA/DVCC. “We provide acute care services for those who have been recently sexually assaulted, have recently left an IPV relationship or are still in an IPV relationship. We also provide follow-up care, which includes Sexually Transmitted Infections testing, counseling services, referrals to internal or external agencies and providing emotional support. But the most important part of our care is that it’s all tailored to the patient – they have the ability to choose or decline any of the options we provide.”
As non-essential hospital services began ramping down across the province, the SA/DVCC remained open. “One of the early challenges we faced was communicating to patients and the community that our services were still available,” described Goulbourne. “This was a priority because we were anticipating an increase in intimate partner violence incidents as people were confined together and experiencing stressors related to the pandemic.”
Anecdotal evidence has shown an escalation in intimate partner violence related to other pandemics. Preliminary studies indicate the same is true for COVID-19 as increased severity and higher incidences of intimate partner violence are being reported worldwide.
The SA/DVCC team quickly reached out to their network of community partners and emergency departments to inform them that nursing staff were still on-site at WCH and the clinic remained open to walk-in patients. They also connected with patients who had follow-up appointments at the Centre to let them know they were still welcome to come in and to advise them about the COVID-19 precautions in place to keep them safe when coming to the hospital.
However, visiting the hospital during a pandemic wasn’t possible for some. “We did get calls where patients experiencing IPV weren’t able to come in to seek services because the abuser was home at all times due to the pandemic. There were fewer excuses to leave their home,” said Kainth. “So you do the best you can to support them in the way that they need, which might not necessarily mean coming in for an appointment. This could be a quick 10-minute phone call over the phone to address any immediate needs.”
Calls to the SA/DVCC continued to increase throughout April. “We started getting over 15 calls a day from individuals just looking for more information on the resources available to them,” explained Goulbourne. “Many patients were also opting for virtual and telephone follow-up visits rather than coming into the centre.”
Phone visits also became a critical tool for the mobile team as the pandemic reduced the SA/DVCC’s ability to visit emergency departments at other hospitals. To minimize the risk of multiple individuals going back and forth between hospitals, the team developed a new patient flow that brings patients to WCH after their emergency department visit or provides the option of telephone support.
“Sometimes our patients are in the emergency departments for a long time. They’re tired, and the fact that they have to go to a second location can seem really exhausting,” described Kainth. “We set up a system where we could do our assessment over the phone, talk to them about their options of care, and then book them into our follow-up clinic.”
However, for some seeking care, there is no place to go after their appointment. “We also have patients coming to us from congregate living spaces or who need to access a shelter,” explained Goulbourne. “Those who present with symptoms or have been in contact with an individual who tested positive for COVID-19 are also tested for the virus as part of their care – a negative result is required to access shelter services.”
Working with internal partners at WCH’s Acute Ambulatory Care Centre, patients are provided with a room and any required care until they receive their COVID-19 results. During their stay, a team of social workers collaborates with Inner City Health Associates to connect the individual with supports and resources, whether it’s a safe place to isolate or a bed in a shelter.
“Even though our patients are coming to us for sexual assault or domestic violence care, we recognized that they may have additional needs,” said Goulbourne. “We are proud that, as a team, WCH is able to provide all aspects of care and ensure nobody gets left behind.”
“We are 24/7, we are drop-in, we are mobile, we are a phone call away. We will ensure that there will always be someone available to provide support.”
Both Goulbourne and Kainth emphasize that cohesive and continuing care throughout the pandemic would not have been possible without a strong network of community and internal partners. The SA/DVCC team supported the Ontario Network of Sexual Assault/Domestic Violence Treatment Centres, which is also housed at WCH, in establishing a 24/7 nurse-staffed navigation phone line that assists both service providers and individuals who have experienced sexual assault or domestic violence. The initiative connected 37 treatment centres from across the province, each committed to supporting the navigation phone line and each other.
“The pandemic created huge challenges for all the sites in terms of remaining accessible to patients,” explained Goulbourne. “The phone line enabled other Centres to step in if a site was being overwhelmed, redirecting patients to the next nearest Centre or linking them with the necessary resources.”
Regardless of the circumstance, all of the Centres strive toward a common goal – that no patient is turned away or goes without care. Beyond the pandemic, Goulbourne sees a continued opportunity for the new streamlined processes and virtual care options to reach patients who live in rural areas or face barriers to accessing in-patient care.
“We want to ensure that we can provide all of our patients with the right resources and care, no matter the circumstances,” Goulbourne said. “We are 24/7, we are drop-in, we are mobile, we are a phone call away. We will ensure that there will always be someone available to provide support.”